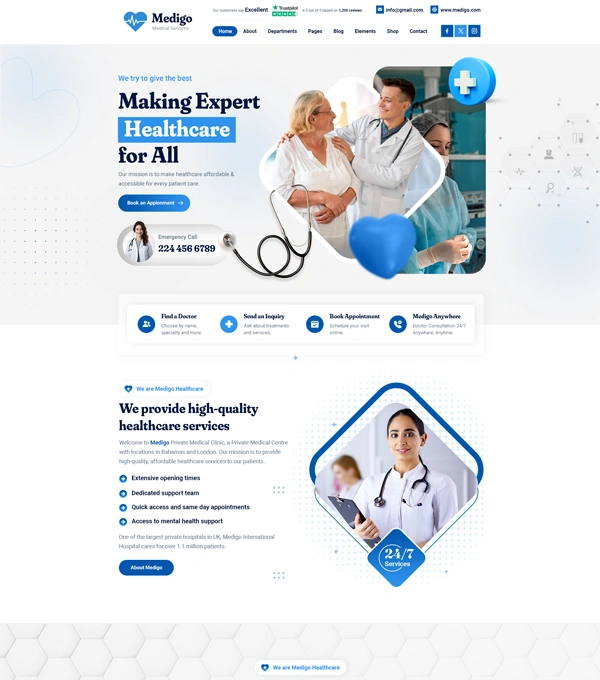
Patient Eligibility in Medical Billing
Patient eligibility verification is a critical first step in the medical billing process. It ensures that the services provided will be covered by the patient’s insurance plan, helping avoid claim rejections, payment delays, and patient dissatisfaction. At Medix Health Claim Billing, we specialize in real-time, thorough eligibility checks to safeguard your revenue cycle from the start.
Clear & Accurate Eligibility Checks
Our team verifies each patient’s insurance coverage details, including plan benefits, deductibles, co-pays, pre-authorizations, and policy status before the date of service. We work closely with healthcare providers to ensure that the right information is collected, verified, and communicated, giving you clarity and control over every patient encounter.


Daily Updates
Accurate eligibility verification not only reduces claim denials but also improves patient transparency, enabling you to set the right financial expectations upfront. Our systemized, proactive approach ensures your administrative staff spends less time chasing insurance information and more time focusing on patient care.
By trusting Medix Health Claim Billing, you can prevent costly mistakes, enhance cash flow, and create a smoother, stress-free experience for both your practice and your patients. Stay ahead with our dedicated eligibility solutions and protect the financial health of your organization.
Why Choose Medix Health Claim Billing for Patient Eligibility?
1st Class Reimbursement:
Swift Reimbursement:
Minimize Denials:
We also provide daily updates on insurance changes and closely monitor payer policies to ensure your records stay current. With Medix, you can confidently deliver services knowing that coverage issues are addressed before they become billing problems. Patient eligibility isn’t just a task—it’s a vital part of your practice’s success, and we’re here to make it effortless.